What to know about pelvic organ prolapse

Pelvic organ prolapse isn’t a topic that tends to come up while chatting with your girlfriends. If you’re experiencing pelvic organ prolapse symptoms, you may not know what could be causing it, or you may feel too embarrassed to talk to your doctor. But there’s no need to feel ashamed about it! Here we share what happens during pelvic organ prolapse and what you can do about it.
In this article
- What is pelvic organ prolapse?
- Are all pelvic organ prolapses the same?
- How common is pelvic organ prolapse?
- What can increase my chances of pelvic organ prolapse?
- Can pelvic organ prolapse affect my reproductive health?
- What are some pelvic organ prolapse symptoms?
- What are the stages of pelvic organ prolapse?
- What should I do if I think I have pelvic organ prolapse?
- What happens if I do have pelvic organ prolapse?
- What can I do to avoid pelvic organ prolapse?
What is pelvic organ prolapse?
First, a quick anatomy lesson: Your pelvic floor, which is made up of muscles, ligaments and tissues, functions like a sling, holding your pelvic organs in place.1 Pelvic organs include the vagina, uterus, bladder, urethra and rectum.1
Pelvic organ prolapse (sometimes referred to as POP) is when your pelvic floor weakens so much that it can no longer hold one or more of your pelvic organs in place. This causes the affected organ(s) to shift or, in more serious cases, to bulge into another organ or extend outside of the vagina.1
Are all pelvic organ prolapses the same?
No. There are several different types of pelvic organ prolapse, including:
- Cystocele (also called anterior vaginal wall prolapse or dropped bladder1): Per the Office on Women’s Health, this type of prolapse occurs “when the bladder drops into or out of the vagina.”2
- Urethrocele: Cleveland Clinic notes that this type of prolapse is caused by weakened pelvic floor muscles, which “can cause the tube that carries pee from your bladder to outside your body (urethra) to droop. A dropped urethra often accompanies a dropped bladder.”1
- Rectocele (also called posterior vaginal wall prolapse or dropped rectum1): The Office on Women’s Health states that this type of prolapse occurs “when the rectum bulges into or out of the vagina.”2
- Uterine prolapse (also called dropped uterus): According to Cleveland Clinic and the Office on Women’s Health, this type of prolapse occurs when the uterus drops down into your vaginal canal, bulging into or out of the vagina.1,2
- Vaginal vault prolapse: According to Cleveland Clinic, this type of prolapse “can cause the top part of your vagina (vaginal vault) to drop into your vaginal canal.”1
- Enterocele: According to Cleveland Clinic, this type of prolapse “can cause your small intestine to bulge onto the back wall or the top of your vagina.”1
The American College of Obstetricians and Gynecologists (ACOG) offers explanations and illustrated videos of different types of pelvic organ prolapses, including those that can occur after a hysterectomy.
How common is pelvic organ prolapse?
Because pelvic organ prolapse doesn’t always cause symptoms, it can be difficult to know how many people are truly affected.1 Sources vary on how many people are affected by, or may be affected by, pelvic organ prolapse. According to the Office on Women’s Health, about 3% of women in the U.S. experience it.2 Additionally, the ACOG states that “women in the United States have a 13% lifetime risk of undergoing surgery for POP.”3
We do know that in the U.S., pelvic organ prolapse occurs more frequently in older women and in white and Hispanic women.2 And while women are at a greater risk, men also can experience pelvic organ prolapse, such as a dropped bladder and/or rectum.1
What can increase my chances of pelvic organ prolapse?
Cleveland Clinic and the Office on Women’s Health identify several different causes of pelvic organ prolapse, including:
- Giving birth vaginally: The risk increases with multiple vaginal births (especially as you get older), giving birth to twins, triplets, etc., and/or giving birth to a baby who weighs more than 8.5 pounds.1,2
- Aging: According to Cleveland Clinic, “the aging process can cause your muscles to lose strength, including your pelvic floor muscles. One factor is declining estrogen. During menopause, your body produces less estrogen. The decline can cause the connective tissues that support your pelvic floor to weaken.”1
- Chronic pressure on the abdomen: This can be due to chronic coughing, constipation or straining during bowel movements, lifting heavy objects frequently, and/or obesity.1,2
- Family history: Research is ongoing, but genetics may play a part, too!1,2
Can pelvic organ prolapse affect my reproductive health?
Pelvic organ prolapse doesn’t directly affect fertility, but it can make having sex more painful, which can make trying to conceive (TTC) more difficult.4 It’s always important to talk to your healthcare provider if you think you may be experiencing pelvic organ prolapse, but communication is especially important if you’re TTC. Healthcare providers often recommend delaying surgical treatment for the condition until you are finished having children.4
Although surgery for pelvic organ prolapse is more common after menopause, the clinical guidance document Female Pelvic Medicine & Reconstructive Surgery notes that an increasing number of younger people are seeking treatment.5 Make sure to talk to your healthcare provider if you’ve been treated for pelvic organ prolapse and are planning to get pregnant.5
What are some pelvic organ prolapse symptoms?
Pelvic organ prolapse can be accompanied by one or several symptoms (though sometimes no symptoms are present1). You may feel surprised, unsettled or even embarrassed by what you’re experiencing. Remember that you are not alone in this experience and that your healthcare provider can help address these symptoms:
- Feeling a general sense of vaginal pressure — or even a bulge — that gets more pronounced as the day progresses, when you cough or if you stand for a long time
- Feeling discomfort in your pelvic area or lower back
- Experiencing pain during sex
- Spotting, which you may notice on your underwear, on toilet paper or in the toilet
- Having to move any protruding organs with your fingers just a bit so you can pee or poop1
If, after reading this list, you’re thinking, I thought I was the only one! — you’re not. That’s why this article exists! But you do need to talk to your healthcare provider. They can discuss the specific symptoms you’re experiencing and go over your treatment options.
What are the stages of pelvic organ prolapse?
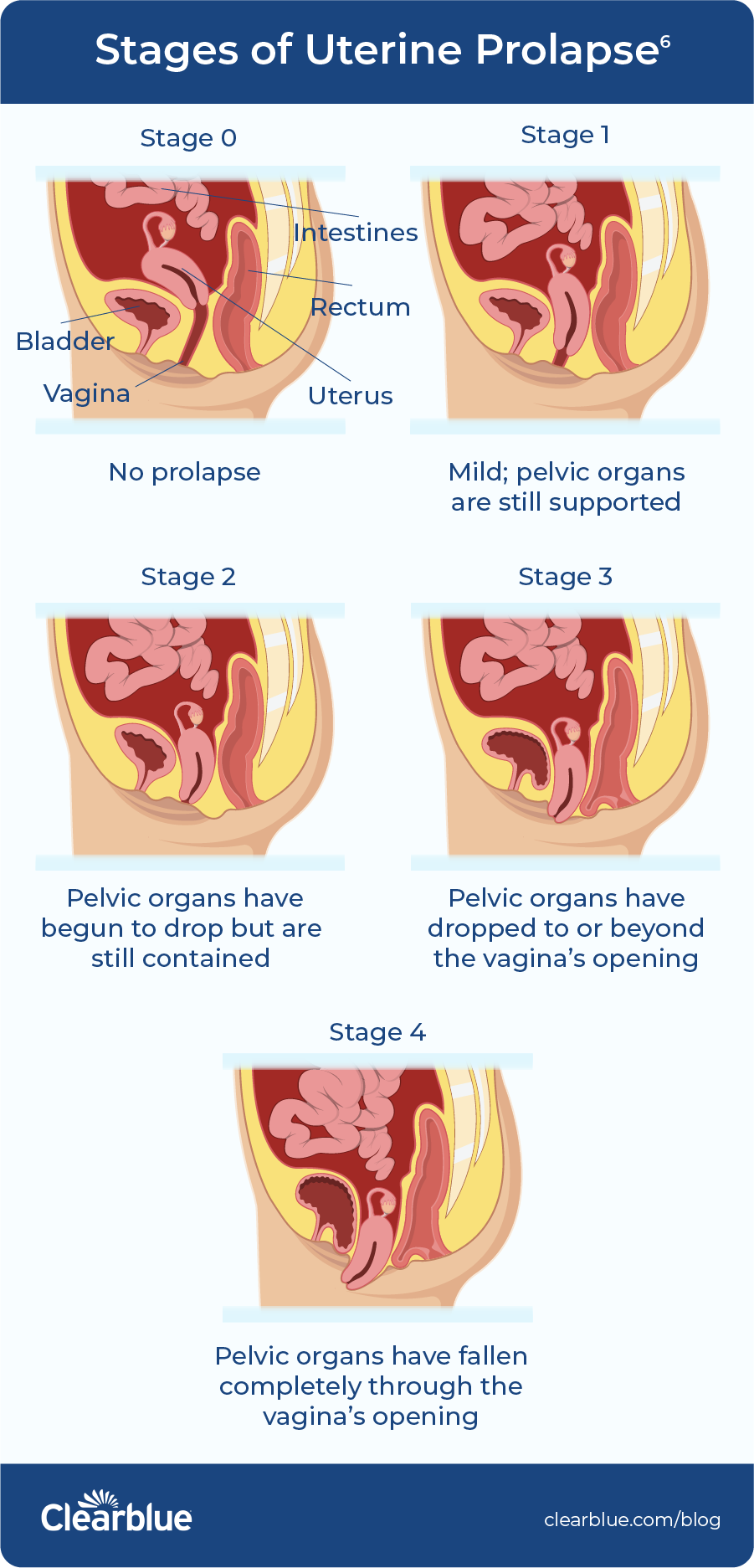
There are four pelvic organ prolapse stages identified by the Pelvic Organ Prolapse Quantification (POP- Q) system;1 this info might come in handy when discussing symptoms with your healthcare provider. According to the National Association for Continence, the stages of pelvic organ prolapse are as follows:
- Stage 1: very mild; pelvic organs are still supported
- Stage 2: pelvic organs have begun to drop but are still contained
- Stage 3: pelvic organs have dropped to or beyond the vagina’s opening
- Stage 4: pelvic organs have fallen completely through the vagina’s opening6
This illustration shows the four stages of uterine prolapse (dropped uterus):
What should I do if I think I have pelvic organ prolapse?
If you think you have pelvic organ prolapse, schedule an appointment with your healthcare provider. You may be shy or embarrassed to make this appointment. Just remember that you are not alone in what you’re experiencing. When the receptionist asks why you wish to be seen, you can simply say, “I think I may have symptoms of pelvic organ prolapse.”
During your appointment, your healthcare provider may perform a pelvic exam to determine if you’re experiencing pelvic organ prolapse.1 Depending on the symptoms you have, your provider may also recommend some tests to rule out or confirm other potential health issues.
What happens if I do have pelvic organ prolapse?
Your healthcare provider will help you determine your next steps based on the type and stage of your pelvic organ prolapse, as well as other factors such as whether you’re finished having children, how uncomfortable your symptoms are and more. According to Cleveland Clinic, “your provider may refer you to a physical therapist to test the strength of individual muscles and teach you targeted exercises [pelvic floor exercises] to train these muscles.1” Your healthcare provider may also recommend a vaginal pessary — a removable silicone device inserted into your vagina designed to help hold your pelvic organs in place.1 Cleveland Clinic also says that “surgery may be an option if your symptoms haven’t improved with conservative treatments and if you no longer wish to have children.”1
What can I do to avoid pelvic organ prolapse?
The National Association for Continence recommends exercises to strengthen your pelvic floor before getting pregnant. Cleveland Clinic offers a list of recommendations to reduce your risk:
- “Do pelvic floor exercises daily.”
- “Maintain a healthy weight.”
- “Prevent constipation.”
- “Don’t smoke.”
- “Protect your pelvic floor when you lift.”1
Pelvic organ prolapse is nothing to feel embarrassed about. If you’re experiencing symptoms, talk to your healthcare provider.
Related Articles
- Cleveland Clinic. Pelvic organ prolapse. Updated August 22, 2022. Accessed May 26, 2023. https://my.clevelandclinic.org/health/diseases/24046-pelvic-organ-prolapse
- Office on Women’s Health, U.S. Department of Health & Human Services. Pelvic organ prolapse. Updated February 22, 2021. Accessed May 26, 2023. https://www.womenshealth.gov/a-z- topics/pelvic-organ-prolapse
- The American College of Obstetricians and Gynecologists. Pelvic organ prolapse. Updated November 2019. Accessed May 31, 2023. https://www.acog.org/clinical/clinical- guidance/practice-bulletin/articles/2019/11/pelvic-organ-prolapse
- Pelvic Awareness Project. Can you get pregnant with pelvic organ prolapse? Updated April 20, 2022. Accessed May 26, 2023. https://pelvicawarenessproject.org/can-you-get-pregnant-with- pelvic-organ-prolapse/
- Wieslander CK, Weinstein MM, Handa VL, Collins SA. Pregnancy in women with prior treatments for pelvic floor disorders. Female Pelvic Med. Reconstr. Surg. 2020;26(5). doi: 10.1097/SPV.0000000000000822. Accessed May 26, 2023. https://www.augs.org/assets/1/6/Pregnancy_in_Women_With_Prior_Treatments_for.4.pdf
- National Association for Continence. Pelvic organ prolapse causes and treatments. Accessed May 26, 2023. https://nafc.org/pelvic-organ-prolapse/

How long is a menstrual cycle?
Most women believe the average menstrual cycle is 28 days long, but cycles can range from 23 to 35 days. Read on to learn more about periods and fertility.

All you need to know about your period
Even if you get your period every month, how much do you really know about periods?




