If you want to deep dive into the science behind Clearblue® Menopause Stage Indicator, you’ve come to the right place. Learn more about how your reproductive hormones change during your life and how Clearblue® Menopause Stage Indicator’s unique smart algorithm uses these changes, alongside other key factors to determine your likely menopause stage*.
Your reproductive journey
You may be surprised to learn that your reproductive journey starts before birth! You’re born with all the ‘eggs’ (or ‘follicles’) that you will need throughout your reproductive life.1 Follicles are individual sacs in the ovary that contain an immature egg. Although your follicles do not fully mature into eggs until puberty, their numbers naturally start to decline from the moment you are born.2
When you reach puberty, you will start getting periods – though for some girls, their periods aren’t that regular. Your reproductive hormones are stimulated and your follicles begin to mature. Whilst you might be having periods, it can take months to years before your ovaries begin to release an egg approximately once every month, a process called ovulation. This repeating process makes up the menstrual cycle, and puberty represents the beginning of your reproductive life.3
Your menstrual cycle
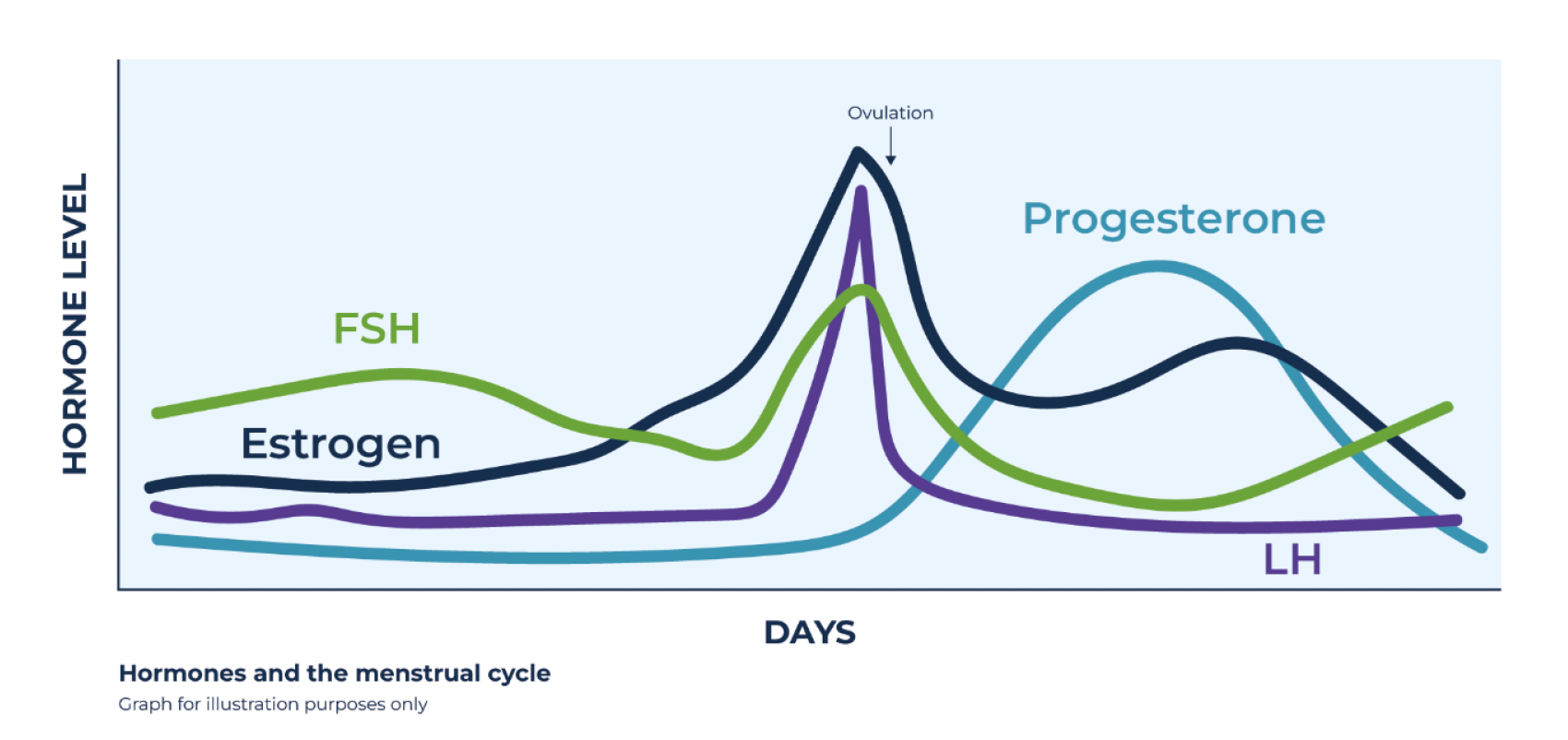
Your menstrual cycle is carefully controlled by a number of important reproductive hormones which work together: Follicle Stimulating Hormone (FSH), Luteinizing Hormone (LH) and the sex hormones estrogen and progesterone. FSH is made in the pituitary gland of the brain, and is responsible for making follicles in the ovary grow and prepare eggs for ovulation. Before puberty, FSH levels are low, so the ovaries do not release any eggs. Around puberty, FSH levels begin to rise and fall at specific points during your menstrual cycle. In the first half of the menstrual cycle, FSH causes follicles to grow. The dominant follicle begins to release estrogen, and when levels are high enough a sudden surge of LH triggers ovulation. After ovulation, the ruptured follicle changes to a corpus luteum which makes progesterone which helps to thicken the womb lining, ready for pregnancy. The sex hormones estrogen and progesterone work together to switch on and off the release of FSH at different times in the cycle.
The menopause transition
As you get older, fewer eggs remain in the ovaries, either due to ovulation or natural loss. This steady loss of eggs over many years is known as reproductive aging and does not necessarily occur at a constant rate for all women. The relatively wide age range for women to reach menopause (typically 42–58 years) suggests that women are either born with a highly variable number of eggs or the rate of egg loss varies greatly.4
You can have many years in the ‘premenopause’ reproductive stage until you start to enter the menopause transition.
The menopause transition marks a period of physiological change as you approach the end of your reproductive life. This is a period of significance for many women as it can be accompanied by a period of noticeable changes in both physical and mental health which can have a negative effect on quality of life.5
The main physiological changes you will experience are to your menstrual cycles and in your reproductive hormones. Perhaps you skipped your period and wondered why? Perhaps your period was a week early or a week late and then next month everything was okay again? Cycles becoming gradually irregular, with the occasional slightly shorter or longer length, (possibly by up to a week or more), are among the first common signs that you are entering early perimenopause.4 Other important symptoms of approaching menopause you may notice include anxiety, mood swings and irritability. As you get closer to menopause, you may start to experience hot flashes and night sweats. As reproductive aging continues and fewer follicles remain in your ovaries, your body produces less estrogen and inhibin B, another hormone. These hormones are usually responsible for suppressing FSH levels.6,7,8 This means that the pituitary gland continues to produce increasing amounts of FSH, as your body attempts to stimulate the remaining follicles to mature. As the number of follicles drops, and the lack of ovarian response to FSH continues, the level of FSH gradually increases and can be measured in either blood, or urine.
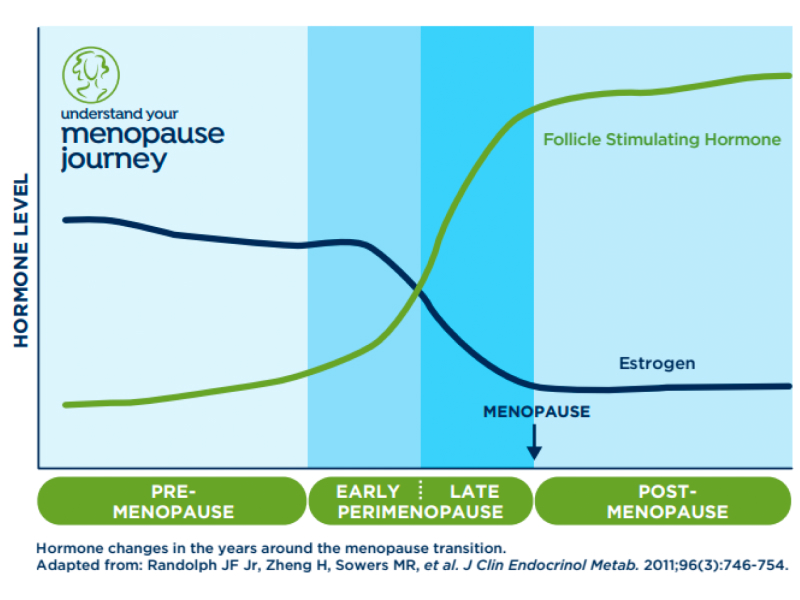
Over time, you will start to notice more frequent irregular cycles and your cycles become much longer (due to a prolonged lack of ovarian response to the raised FSH), maybe frequently skipping your periods and going for as long as two, three months or more, which is typical of progression into late perimenopause.4
Eventually, when all your eggs have been exhausted, you will have your final menstrual period, and menopause can be diagnosed by a healthcare professional retrospectively, 12 months after your last menstrual bleed. Menopause is therefore only a single day. The stage following this day is postmenopause, with complete absence of ovarian activity or menstrual cycles, during which FSH levels remain continually raised. You will remain in postmenopause for the remainder of your life.
These changes in your cycles alongside the gradual increase in FSH over time, and your age are used by Clearblue® Menopause Stage Indicator smart algorithm to scientifically indicate your likely menopause stage*.
How is your menopause stage indication determined?
The Clearblue® Menopause Stage Indicator uses two important physiological indicators as factors in the smart algorithm; your cycle history and FSH hormone levels in your urine. These two factors are in line with the STRAW+10 staging system which is an internationally recognized reference method for characterizing reproductive aging through menopause.4 The smart algorithm also uses your age, so when all three factors are combined, an indication of your most likely menopause stage* is given, together with tailored result messaging and next steps specific to you. Let’s explore these important factors a little more…
Is Clearblue® Menopause Stage Indicator right for me?
Take our simple quiz to find out!
Factor #1. Menstrual cycle variability
When you set up your account you are asked a few important questions about your cycle history over the last 12 months. This is to establish what your cycles have been like and whether your periods have been regular, irregular or if they have stopped completely. By looking at the changes and the extent of those changes in your cycle patterns the smart algorithm uses this information, combined with your FSH levels and age, to determine your likely stage*.
Factor #2. FSH hormone levels
Follicle Stimulating Hormone (FSH) is a key hormone which can be used to track the menopause journey so that is why we test for it with our 5 FSH test sticks. In order to most accurately determine your overall FSH level, we ask you to take 5 tests, first thing in the morning, on alternate days, starting whenever is convenient for you.
Factor #3. Age
The third factor used is age which is an important indicator to help determine likely menopause stage, with average age of menopause, 51 years.
Your Menopause Stage Indicator result
The smart algorithm uses your cycle information, FSH results and age to provide you with your likely menopause stage*. You can generate a personalized report to share with your healthcare professional, which includes your likely menopause stage*, how it was determines and up to 6 weeks of tracked symptoms.
* Only a healthcare professional can confirm your menopause stag
- Peters H, Byskov AG, Grinsted J (1978) Follicular growth in fetal and prepubertal ovaries of humans and other primates. Clin Endocrinol Metab 7:469-85
- Lintern-Moore S, Peters H, Moore GPM, Faber M (1974) Follicular development in the infant human ovary. J Reprod Fert 39:53-64
- Richard E. Jones PhD, Kristin H. Lopez PhD, in Human Reproductive Biology (Fourth Edition), 2014
- Michael R. Soules, M.D., et al. Executive summary: Stages of Reproductive Aging Workshop (STRAW) FERTILITY AND STERILITY_VOL. 76, NO. 5, NOVEMBER 2001
- Harlow SD, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. J Clin Endocrinol Metab. 2012;97(4):1159-1168.
- https://prod.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/menopausal-transition-perimenopause-what-is-it/ (accessed 25th July 2023)
- N A Klein, et al. Decreased inhibin B secretion is associated with the monotropic FSH rise in older, ovulatory women: a study of serum and follicular fluid levels of dimeric inhibin A and B in spontaneous menstrual cycles. J Clin Endocrinol Metab 81:2742-5
- Shaw, N. D., et al. (2010). Estrogen negative feedback on gonadotropin secretion: evidence for a direct pituitary effect in women J Clin Endocrinol Metab. 2010 Apr;95(4):1955-61

Get a personalized menopause report to share with your doctor!
Generate a personalized report with Clearblue® Menopause Stage Indicator including likely menopause stage, FSH results and up to 6 weeks of tracked symptoms


