
Menopause is a natural part of the aging process, but sometimes the symptoms you may get before, leading up to, or after menopause can interfere with daily life. Your healthcare professional can help you confirm if this is due to menopause or something else, and find the right treatment to manage any uncomfortable symptoms or medical issues you may have.
Read on to learn a little more about some of the treatment options your healthcare professional may recommend to help with your menopause journey.
Hormone replacement therapy (HRT)
Hormone replacement therapy (HRT) is the most commonly prescribed treatment for typical perimenopause symptoms, generally caused by the declining levels of estrogen. These symptoms include vasomotor symptoms such as hot flashes and night sweats but HRT can also help prevent bone loss or fractures.1
HRT can take the form of:
- pills
- skin patches
- sprays
- gels
- implants that release hormones into the body
HRT uses hormones like estrogen or progestogens (including progesterone) that either are the same or similar to those naturally produced by your body. HRT works by replacing your body’s declining estrogen levels, while progesterone is added to prevent ‘estrogen dominance’ in women who still have a womb. This treatment can help reduce the symptoms caused by menopause related hormone changes.2
Only a healthcare professional can prescribe HRT and your suitability depends on your personal circumstances. Talk to your healthcare professional to find out more.
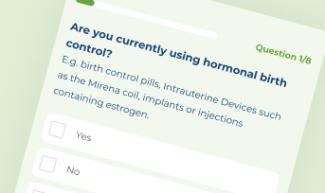
Is Clearblue® Menopause Stage Indicator right for me?
Take our simple quiz to find out!
Non-hormonal medical options
There are other prescription therapies a healthcare professional might recommend to help manage menopause symptoms if HRT is not an option. Paroxetine mesylate and fezolinetant have been approved by the FDA to treat vasomotor symptoms. Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are prescribed to treat anxiety and depression however, they have also been shown to have moderate improvements on vasomotor symtoms.4 Speak to your healthcare professional as they will be able to provide you with your best options based on your personal history and circumstances.
Vaginal treatment
Vaginal dryness is not only uncomfortable, but it can get in the way of your sex life. It can make sex painful, but can be treated using hormones. However, the hormone treatments used to treat vaginal dryness are given via a cream or even a simple vaginal moisturizer. Options can include:
- Vaginal estrogen therapy - this is a cream with low-dose estrogen that you apply to your vagina. It can help rebuild tissue and also moisturizes the vagina walls. Since very little estrogen enters the bloodstream, this may be a good alternative for women who don’t want to take HRT as the side effects are much lower.2
- Vaginal moisturizers - you can also try an over-the-counter vaginal moisturizer, which can help restore some of the original moisture in the vagina.
- Water-based lubricants - if you suffer from pain during sex you may want to use a water-based lubricant to help reduce friction and discomfort.3
Therapy (such as Cognitive behavioral therapy (CBT))
If you’re feeling low or anxious, your healthcare professional may recommend cognitive behavioral therapy (CBT). This is a type of talking therapy that can help with some of the psychological issues associated with the menopause journey, such as feeling low or having anxious thoughts.5 Sometimes it can even help with insomnia.6 Your healthcare professional can help you figure out if CBT might be a good option for you.
Vitamin D and calcium supplements
If you have entered the postmenopause stage of your journey, then osteoporosis, a skeletal condition which weakens your bones7, is one of your main health risks, again due to reduced estrogen, which is essential for bone health. However, you can do your bit to help reduce your chance of bone fractures by ensuring an intake of 1,200 mg/day calcium and 400-600 IU/day vitamin D.8
Sources of calcium and vitamin D include dairy products, dark green leafy vegetables and fortified foods such as soy products and cereals.9 Calcium and vitamin D supplements are also widely available however a healthy women should not need supplements as the RDA for vitamin D is 600 IU to 800 IU daily and daily intakes of 1,000 IU to 2,000 IU will usually ensure vitamin D adequacy for women at risk for osteroprosis.10 Always speak to your healthcare professional before taking any supplements to understand if they are right for you.
- https://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/ART-20046372 (accessed 27th June 2023)
- http://www.menopause.org/for-women/expert-answers-to-frequently-asked-questions-about-menopause/hormone-therapy-menopause-faqs (accessed 4th May 2023)
- https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/diagnosis-treatment/drc-20352294 (accessed 4th May 2023)
- The 2023 nonhormone therapy position statement of The North American Menopause Society. (2023). Menopause (New York, N.Y.), 30(6), 573–590. https://doi.org/10.1097/GME.0000000000002200
- CBT may be effective in managing menopause symptoms (medicalnewstoday.com) (accessed 4th May 2023)
- http://www.menopause.org/publications/clinical-care-recommendations/chapter-3-clinical-issues (accessed 4th May 2023)
- https://www.nia.nih.gov/health/osteoporosis (accessed 4th May 2023)
- North American Menopause Society (2006). The role of calcium in peri- and postmenopausal women: 2006 position statement of the North American Menopause Society. Menopause (New York, N.Y.), 13(6), 862–880. https://doi.org/10.1097/01.gme.0000243566.25205.0b
- https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/calcium-supplements/art-20047097 (accessed 27th Jun 2023)
- 10. McClung, M.R. (2022) ‘Should vitamin D supplements be prescribed routinely for midlife women?’, Menopause, 29(11), pp. 1329–1330. doi:10.1097/gme.0000000000002066.

Get a personalized menopause report to share with your doctor!
Generate a personalized report with Clearblue® Menopause Stage Indicator including likely menopause stage, FSH results and up to 6 weeks of tracked symptoms



