What to expect in perimenopause

What can you expect during the perimenopause years leading up to menopause? Read on for some broad guidelines about perimenopause — and be sure to talk to your healthcare professional for medical advice on what’s best for your health.
In this article
- What is perimenopause?
- How long does perimenopause last?
- What are the signs of perimenopause?
- How can you manage perimenopause symptoms?
- What about perimenopause supplements?
- Is there an ideal perimenopause diet?
- What if you’re trying to conceive in perimenopause?
- What are symptoms of ovulation during perimenopause?
- What are signs perimenopause is ending?
What is perimenopause?
Perimenopause is the time of transition between your reproductive years and menopause.1 The word “perimenopause” means “around menopause.”2
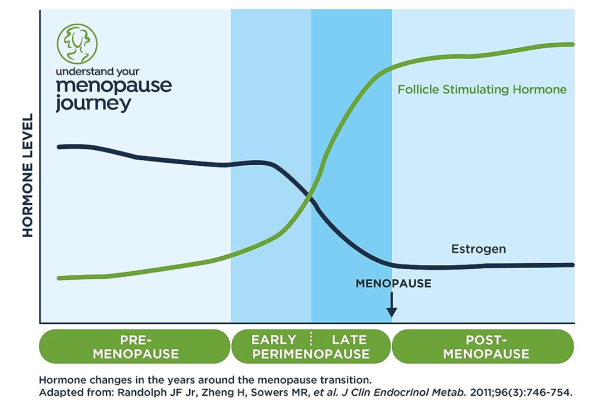
Perimenopause is a two-stage event that begins when the production of estrogen and progesterone in your ovaries begins to decline.1,3 You’re likely in early perimenopause if you notice that over the last year, your menstrual cycles have often varied in length by seven days or more.3 This is caused by fluctuating follicle stimulating hormone (FSH) levels.4 You’re likely in late perimenopause if you have a space of 60 days or more between your periods.3 Late perimenopause typically can last between one and three years.3
During late perimenopause, the menstrual cycles become more irregular in length.3 As you can see in the chart below, hormone levels, including estrogen and FSH, also go through extreme changes.3 FSH levels will become steadily elevated,4 while estrogen levels will decline.
You also have more cycles where you don’t release an egg at all, which is called anovulation.3 (Note: Although irregular menstrual cycles are a common sign of perimenopause, it’s important to report any abnormal bleeding to your healthcare professional.5)
Menopause is a one-day event that occurs when you’ve gone a full year — 12 consecutive months — without having a period.1 After menopause you are considered in postmenopause.1 Note that if you are using hormonal birth control, you may not have any periods. However, this doesn’t necessarily mean you are postmenopausal; a lack of periods may be due to your usage of hormonal birth control.6
According to The Menopause Society (formerly known as the North American Menopause Society, or NAMS), menopause most typically occurs in your early 50s (on average at age 51), though it can occur anytime between the ages of 40 to 58.7 This wide age range means that there’s a similarly wide range of ages when perimenopause can begin, though according to the U.S. Office on Women’s Health, it typically starts in your mid-to-late 40s.2
If menopause is induced, you may not experience perimenopause. Induced menopause can occur if the ovaries are surgically removed, or during certain treatments such as chemotherapy or radiation around the pelvic area.7
How long does perimenopause last?
There is no consensus on how long perimenopause typically lasts — it can be anywhere from 2-14 years.1,2 According to the Office on Women’s Health, the average duration is four years,2 while the National Institute on Aging says it usually lasts around seven years but can be as long as 14 years.1
Remember, menopause doesn’t happen until one full year after your final period and is a single day. Perimenopause includes the time after the onset of lower estrogen and progesterone production (and the resulting period irregularity) and lasts up until the end of that full year with no periods at all.
Is Clearblue® Menopause Stage Indicator right for me?
Take our simple quiz to find out!
What are the signs of perimenopause?
If you are going through perimenopause, you may experience a number of symptoms — or no symptoms at all beyond a change in your cycle. The symptoms you experience may or may not vary from those your friends experience.7 Some of the common symptoms of perimenopause can include:
With all these varying symptoms, how on earth do you know if what you’re experiencing is related to perimenopause? In addition to your age, pay attention to one of the most telling signs: changes in your menstrual cycle. This could include the length of your periods, how much you bleed and how often you have your periods.2,5,7 That said, abnormal bleeding could also be a sign of a different health issue.5 So if you begin to experience changes in your menstrual cycle, talk to your healthcare professional.
How can you manage perimenopause symptoms?
If you have symptoms that are bothersome, it’s important to talk to your healthcare professional about any options that might work for you.8 There are certain things you may be able to do to help manage the symptoms of perimenopause, such as exercising, limiting your alcohol intake and not smoking.9 Strengthening your pelvic floor may help with urinary incontinence.10 If you are struggling with mood issues or depression, talk to your healthcare professional about the best options for you.10
What about perimenopause supplements?
A quick search online will lead you to dozens of supplements offering “miracle cures” for uncomfortable perimenopause and menopause symptoms — but as always, you should talk to your healthcare professional before considering adding any supplements to your routine.
Black cohosh has been purportedly used for everything from hot flashes to vaginal dryness, but studies on its efficacy are mixed — and there are some safety concerns with taking it, particularly related to liver health.11,12 Soy, red clover and flaxseed are also popular supplements, but the research on these is also mixed.13,14
It’s also important to note that the manufacture of these products is not regulated. According to The Menopause Society, “Few OTC therapies have the patient package insert that provides vital information on the safety and effectiveness of the drug, information that is required by the U.S. Food and Drug Administration (FDA) for all prescription medications. Because the normal regulations for prescription or OTC drugs do not apply to dietary supplements, demonstrating safety is not required before a dietary supplement is put on the market.”15 If you’re looking for help managing perimenopause symptoms, talk to your healthcare professional about safety, options and whether to try a supplement as part of your management plan. It’s also important to talk to your healthcare professional if you’re already taking supplements in response to perimenopause symptoms.
Is there an ideal perimenopause diet?
There is no singular diet that’s best for everyone during this transitional time. That said, some interesting studies have recently been conducted on the matter, especially on how dietary changes can impact symptoms. While there’s nothing conclusive, below are the results of some of these studies.
- A 2021 study showed that a plant-based diet rich in whole soybeans reduced moderate-to-severe hot flashes by 84%. Participants ate a low-fat, vegan diet and consumed a half-cup of cooked whole soybeans daily.16
- A 2022 study showed that focusing on increasing the amount of protein you eat while also decreasing the amount of carbohydrates and fats can ward off weight gain during perimenopause. And the best part? Only minor adjustments made to individuals’ daily diets were needed to make a difference.17
- A 2022 study showed merit in eating a Mediterranean diet — legumes and extra virgin olive oil seemed to lessen perimenopausal symptoms.18
What if you’re trying to conceive in perimenopause?
Fertility is different for everyone, but knowing when you ovulate during perimenopause can be difficult because fertility begins to gradually decline in your 30s, before perimenopause even begins. It’s a good idea to talk to your healthcare professional when you’re trying to conceive. It’s especially important to talk to your healthcare professional if you’re under 35 and have been trying to get pregnant for a year, over 35 and have been trying for six months or right away if you’re 40 or older.19
What are symptoms of ovulation during perimenopause?
Whether you’re trying to conceive or not, the signs of ovulation are the same as when you were younger. The tricky thing about perimenopause is that you may not ovulate every cycle. Many women use fertility-awareness-based methods to track ovulation but these methods are not reliable enough during the unpredictable period of perimenopause. Ovulation tests which work by identifying the rise in hormones that surge just before you release an egg, may help you know if and when you’re ovulating during perimenopause. But since long and irregular cycles are common during perimenopause, ovulation tests may not be suitable. If you want to conceive and you suspect you’re in perimenopause, it’s important to see your healthcare professional right away.
Ovulation — and pregnancy — are still possible during perimenopause. If you’re not trying to conceive, The Menopause Society recommends using birth control until you reach menopause simply because ovulation can be so unpredictable during this time.6
What are signs perimenopause is ending?
Perimenopause officially ends once you’ve gone 12 consecutive months without having a period. Menopause occurs for one day, and then postmenopause begins. However, there’s no consistently clear symptom or sign it will be ending soon.
If you start noticing longer times between your menstrual cycles, that could be a sign perimenopause is ending.20 Your healthcare professional will confirm perimenopause has ended and you have transitioned into postmenopause after you haven’t had a period in 12 months. According to The Menopause Society, in perimenopause, testing for FSH only one time can be misleading because estrogen production and FSH levels vary greatly during this time.21
Just like puberty, perimenopause signifies a shift in your life. Be gentle with yourself. One of the most helpful and powerful tools in your arsenal? Friends and family members who are going through perimenopause with you or have gone through it already. By sharing your experiences, you can learn what has helped others and know you are far from alone.
Related Articles
Sources
- National Institute on Aging. What is menopause? Updated September 30, 2021. Accessed January 31, 2023. https://www.nia.nih.gov/health/what-menopause
- Office on Women’s Health, U.S. Department of Health & Human Services. Menopause basics. Updated January 6, 2023. Accessed January 31, 2023. https://www.womenshealth.gov/menopause/menopause-basics
- Harlow SD, Gass M, Hall JE, et al. Executive summary of the stages of reproductive aging workshop+ 10: addressing the unfinished agenda of staging reproductive aging. Menopause. 2012;19(4). doi: 10.1097/gme.0b013e31824d8f40. Accessed March 20, 2023. https://www.menopause.org/docs/default-document-library/straw10.pdf?sfvrsn=67b7c029_2
- Hotspex menopause incidence survey Feb’22. 1022 US women, age 35-60. Quantitative online survey. ACOG Practice Bulletin No. 141: management of menopausal symptoms. Obstet Gynecol. 2014 Jan;123(1):202-216. doi: 10.1097/01.AOG.0000441353.20693.78. Accessed April 11, 2023. https://journals.lww.com/greenjournal/abstract/2014/01000/practice_bulletin_no__141__management_of.37.aspx
- The American College of Obstetricians and Gynecologists. The menopause years. Updated November 2021. Accessed January 31, 2023. https://www.acog.org/womens-health/faqs/the-menopause-years
- The North American Menopause Society. Contraception: you need it longer than you may think. Accessed February 2, 2023. https://www.menopause.org/for-women/sexual-health-menopause-online/reminders-and-resources/contraception-you-need-it-longer-than-you-may-think
- The North American Menopause Society. Menopause 101: A primer for the perimenopausal. Accessed January 5, 2023. https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal
- Cleveland Clinic. Perimenopause. Updated October 5, 2021. Accessed January 5, 2023. https://my.clevelandclinic.org/health/diseases/21608-perimenopause#management-and-treatment
- National Health Service. Menopause — things you can do. Updated May 17, 2022. Accessed August 16, 2023. https://www.nhs.uk/conditions/menopause/things-you-can-do
- The North American Menopause Society. Five solutions for menopause symptoms. Accessed January 5, 2023. https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/five-solutions-for-menopause-symptoms
- Office of Dietary Supplements, National Institutes of Health, U.S. Department of Health & Human Services. Black cohosh. Updated June 3, 2020. Accessed January 31, 2023. https://ods.od.nih.gov/factsheets/BlackCohosh-HealthProfessional/
- National Center for Complementary and Integrative Health, National Institutes of Health, U.S. Department of Health and Human Services. Menopausal symptoms and complementary health approaches: what the science says. Updated February 2021. Accessed January 31, 2023. https://www.nccih.nih.gov/health/providers/digest/menopausal-symptoms-and-complementary-health-approaches-science#soy
- Franco OH, Chowdhury R, Troup J, et al. Use of plant-based therapies and menopausal symptoms: a systematic review and meta-analysis. JAMA. 2016;315(23):2554-2563. doi: 10.1001/jama.2016.8012. Accessed January 31, 2023. https://jamanetwork.com/journals/jama/fullarticle/2529629
- Griffin RM, WebMD. Flaxseed. Updated April 26, 2023. Accessed August 14, 2023. https://www.webmd.com/a-to-z-guides/supplement-guide-flaxseed-oil
- The North American Menopause Society. Menopause symptoms FAQ. Accessed August 14, 2023. https://www.menopause.org/for-women/expert-answers-to-frequently-asked-questions-about-menopause/menopause-symptoms-faqs
- Barnard ND, Kahleova H, Holtz DN, et al. The women’s study for the alleviation of vasomotor symptoms (WAVS): a randomized, controlled trial of a plant-based diet and whole soybeans for postmenopausal women. Menopause: The Journal of the North American Menopause Society. 2021;28(10):1150-1156. doi: 10.1097/GME.0000000000001812. https://journals.lww.com/menopausejournal/Fulltext/2021/10000/The_Women_s_Study_for_the_Alleviation_of_Vasomotor.12.aspx
- Simpson SJ, Raubenheimer D, Black KI, Conigrave AD. Weight gain during the menopause transition: evidence for a mechanism dependent on protein leverage. BJOG. 2023;130(1):4-10. doi: 10.1111/1471-0528.17290. Accessed January 31, 2023. https://obgyn.onlinelibrary.wiley.com/doi/10.1111/1471-0528.17290?af=R
- Vetrani C, Barrea L, Rispoli R, et al. Mediterranean diet: what are the consequences for menopause? Front Endocrinol (Lausanne). 2022;13:886824. doi: 10.3389/fendo.2022.886824. https://www.frontiersin.org/articles/10.3389/fendo.2022.886824/full
- The American Society for Reproductive Medicine. Age and fertility. Accessed January 5, 2023. https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/age-and-fertility-booklet/
- Cleveland Clinic. How to tell you’re near the end of perimenopause. Updated October 17, 2022. Accessed January 31, 2023. https://health.clevelandclinic.org/signs-perimenopause-is-ending/
- The North American Menopause Society. How do I know when I’m in menopause? Accessed January 5, 2023. https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/how-do-i-know-when-i'm-in-menopause-

Know more about the menopause journey
Download the Menopause Stage - Clearblue® me app to access relevant educational content, track your symptoms & periods




