Top questions about menopause to ask your healthcare professional

Maybe you’ve been having hot flashes (who knew how suddenly they could show up?!). Or your anxiety has been sky high lately. Or you’ve been experiencing pain during sex. Based on what you’ve heard from friends, your mom or the internet, you may start to wonder: Could this be it — the start of menopause?
It could be! Which is exactly why you should schedule an appointment with your healthcare professional as soon as you can. Here we share general tips and considerations for discussing this important topic with a professional who knows you and your unique health circumstances.
Which healthcare professionals treat menopause?
Primary care physicians (PCPs), including those in family medicine and internal medicine, may be able to address broad concerns you have about menopause. Or your primary care physician might direct you to a more specialized healthcare professional, such as a gynecologist or an endocrinologist.
The reality is that your day-to-day healthcare professional may not have received specific menopause care training. A 2023 study published in Menopause magazine looked at the results of a 2022 survey emailed to 145 U.S. ob-gyn residency program directors (PDs). Of the 99 out of 145 PDs who responded, 92.9% “strongly agreed that residents nationwide should have access to a standardized menopause curriculum that could be utilized in their programs,” but only 31.3% reported “having a menopause curriculum in their residency program.”1
So, where does this leave you? The Accreditation Council for Continuing Medical Education has accredited the Menopause Society to certify healthcare professionals who have undergone advanced training specifically related to menopause.2 The Menopause Society’s Find a Menopause Practitioner directory is a useful tool if you are looking for a local certified menopause specialist.
How can you help make sure your menopause care is a positive experience?
In survey results published in 2023 in the Journal of Women’s Health, 964 respondents answered the open-ended question “How did that go?” regarding their experiences seeking healthcare for symptoms related to perimenopause.3 Forty-nine percent of those who responded reported experiences the researchers perceived as “negative or dissatisfying,” whereas only 18% reported experiences the researchers perceived as “positive or satisfying.”3 Some of the experiences that women perceived as “invalidating” included comments like these:
- “It’s not hormonal. You’re too young and healthy and have normal periods.”3
- “I was told it was part of life.”3
- “[I]t didn’t go well. [T]hey told me it was because I had teenage kids and a career and not because of my hormones even though I’m positive that’s the reason.”3
In contrast, positive “validating” experiences included comments like these:
- “It went well. My doctor made me feel heard and supported.”3
- “She said it could be perimenopause. I felt she understood where I was at and let me know other patients of hers are going [through] the same things. So I wasn’t alone.”3
- “In discussing symptoms with both my gynecologist and PCP, we decided to address my anxiety with exercise, meditation and diet, and will revisit with both providers at my annual checkups.”3
Try to go into this conversation with an empowered mindset. As you’re sharing your symptoms and asking questions, remind yourself that this is your allotted time. The goal here is mutual understanding. If you feel as if you aren’t being listened to, repeat and restate. If your questions aren’t being answered, ask again. (Also, come prepared! See the list of suggested questions below, which you may find helpful and can bring to the appointment.) Ask follow-up questions. You should leave your appointment feeling as if you and your healthcare professional are on the same wavelength. If, at the end of your appointment, you don’t feel as if you were taken seriously or listened to, you always have the option of seeking a second opinion.
How do I know if it’s menopause?
Only a healthcare professional can confirm a menopause stage diagnosis. The Clearblue® Menopause Stage Indicator helps you understand your menopause journey by providing an indication of your likely menopause stage.4
Here’s how it works:
- The hormone FSH (follicle stimulating hormone) rises as you get closer to menopause.
- The Clearblue® Menopause Stage Indicator uses 5 urine tests to track this key hormone over several days in a free-to-download app.5
- The Smart Algorithm in the app combines the results with your cycle history and age to determine your likely menopause stage:4 Premenopause, Early perimenopause, Late perimenopause or Postmenopause.
The results from the Clearblue® Menopause Stage Indicator can enable more effective and empowered conversations when talking about menopause with your healthcare professional. In addition to giving you the ability to track cycles and both the frequency and intensity of your symptoms, the Clearblue® Menopause Stage Indicator also provides in-app educational content and a downloadable, personalized report for you to print and take to your healthcare professional.
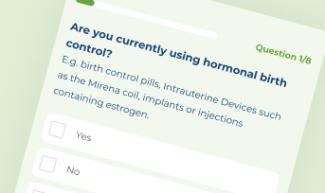
Is Clearblue® Menopause Stage Indicator right for me?
Take our simple quiz to find out!
What questions about menopause should you ask your healthcare professional?
You will likely have questions specific to symptoms you may be experiencing. However, it can be easy to get sidetracked or forget some questions in the moment.
Also, you may not have had a lot of exposure to menopause — and that’s OK! You’re definitely not alone. According to a 2022 study in Women’s Health, over 90% of respondents said they “had never been taught about menopause at school,” and over 60% didn’t feel knowledgeable about menopause “at all.”6 Having limited exposure can make it difficult to know what to ask, which is why we’ve tried to make things a bit easier for you. Take a look at this general list of questions and feel free to remove any that don’t pertain to you or add your own. This is your list.
How will I know I’m getting close to menopause?
- What is perimenopause
- What are the different stages of menopause and how do I know which one I’m in?
- I’m experiencing [X, Y, Z] symptoms. Could these symptoms be related to perimenopause?
- What if I don’t experience any symptoms at all? How will I know if perimenopause has begun?
- I’ve taken an FSH test. Can you review and confirm my results and suggest the next best steps?
Can you help me manage my symptoms?
- How do we determine if these symptoms are related to perimenopause or something else?
- What can I do to improve my quality of life right now?
- What are some practical ways to manage, for example, hot flashes at work? What about ones at night? And they keep getting worse — how do I alleviate that? (In other words, be specific about the symptoms you’re experiencing!)
- What are the advantages and disadvantages of a holistic approach to treating the symptoms of menopause versus medication to managing menopause symptoms?
- How effective are some of the most recent treatments?
- What are the benefits, risks, side effects and costs (if any) associated with this next course of action?
- What perimenopause symptoms may develop in the future?
- What should I do if I notice a new symptom?
- What should I do if a symptom becomes worse over time?
Additional questions
- What is your last period typically like before menopause?
- As I get older, how can I ensure good overall health? Will doing so help lessen my perimenopause symptoms?
- How long is all of this going to last?
Pause for a moment and think about all the things your body has been through over the course of your life. We’ve all had beautiful, heartbreaking or significant reproductive health experiences that have carried us to where we are today. This journey matters, too. Your perimenopause symptoms matter. When talking with your healthcare professional about the stages of menopause, don’t be shy about speaking up and making sure your voice is heard loud and clear.
Related Articles
Sources and Disclaimers
- Allen JT, Laks S, Zahler-Miller C, Rungruang BJ, Braun K, Goldstein SR, Schnatz PF. Needs assessment of menopause education in United States obstetrics and gynecology residency training programs. Menopause. 2023;30(10):1002-1005. doi: 10.1097/GME.0000000000002234. Accessed August 17, 2023. https://journals.lww.com/menopausejournal/abstract/9900/needs_assessment_of_menopause_education_in_united.225.aspx
- The Menopause Society. NAMS CME. Accessed August 17, 2023. https://www.menopause.org/forprofessionals/nams-cme
- Richardson MK, Coslov N, Fugate Woods N. Seeking health care for perimenopausal symptoms: observations from the women living better survey. Journal of Women’s Health. 2023;32(4):434-444. https://doi.org/10.1089/jwh.2022.0230. Accessed August 17, 2023. https://www.liebertpub.com/doi/10.1089/jwh.2022.0230
- Only a healthcare professional can confirm your menopause stage.
- Compatible with most iPhones® and Android™ Phones. To find out if your phone is compatible and if the app is available in the country you live in, check out: www.clearblue.com/connectivity.
- Harper JC, Phillips S, Biswakarma R, Yasmin E, Saridogan E, Radhakrishnan S, Davies MC, Talaulikar V. An online survey of perimenopausal women to determine their attitudes and knowledge of the menopause. Women’s Health. 2022;18. doi: 10.1177/17455057221106890. Accessed August 17, 2023. https://journals.sagepub.com/doi/10.1177/17455057221106890

What’s your menopause stage?
The menopause journey has stages. Learn about yours with Clearblue® Menopause Stage Indicator – 5 easy-to-use tests & a FREE app.

Can I get pregnant if I'm over 35?
If you’re over 35 you may need a little more patience and greater understanding about your fertility window to help you have a baby naturally.





