Getting pregnant with low sperm count?: How oligospermia can affect fertility
Low sperm count (also called oligospermia or oligozoospermia), is a common cause of male fertility problems and can be challenging for couples trying to conceive naturally. While having a successful pregnancy is still possible, it might take longer or require certain treatments or procedures. Here, we share some information for trying to get pregnant with low sperm count.
What is low sperm count and why does it happen?
Fewer than 15 million sperm in 1 mL of semen is considered low sperm count.1 According to the Urology Care Foundation, sperm problems can result from traits you’re born with, lifestyle choices, childhood infections, long-term sickness, medications, chromosome or hormone problems.2
Some causes of low sperm count include:
- Varicoceles: Found in 16 out of every 100 men (and in 40 out of every 100 infertile men), these swollen veins in the scrotum disrupt blood flow and can overheat the testes, lowering sperm production.2,3
- Hormones: Low hormone levels in the pituitary gland can cause poor sperm growth.2
- Medications: Certain medications used to treat arthritis, digestive problems, anxiety or depression, infections, high blood pressure and cancer can cause low sperm count.2 Talk to your healthcare provider for more information.
- Sexually transmitted diseases: Gonorrhea and chlamydia can cause the testicles to swell, resulting in low sperm count.4
- Chromosome anomalies: Klinefelter syndrome, in which men have an extra X chromosome, is the most common chromosomal cause of male infertility.5 Men with cystic fibrosis may have an anatomical condition called congenital bilateral absence of the vas deferens (CBAVD), which results in a lack of sperm in semen and may cause thinner ejaculate and lower semen volume.6 Also, a genetic condition called Y chromosome infertility, caused by changes to the Y chromosome in men, can cause low sperm count as well.7
- Injury to the testicle: Testicles hang outside the body, so they can be damaged more easily. According to the Urology Care Foundation, testicular trauma is when a testicle is hurt by force. That trauma to the testicle or scrotum can reduce sperm count.4,8
- Thyroid problems: Hyperthyroidism is associated with low sperm count.4,9
- Lifestyle factors: A 2021 meta-analysis of 44 studies of 20,367 obese patients, 1,386 of whom had diabetes, showed that patients who were both obese and had diabetes were associated with low sperm count.10 Alcohol, tobacco and marijuana use have also been associated with low sperm count.2,11
- Environmental toxins: Exposure to air pollution, certain insecticides, BPA and some heavy metals have been associated with low sperm count.11
- Radiation therapy: Cancer treatments that require radiation therapy can destroy sperm cells and the stem cells that make sperm.12 Folks who are undergoing cancer treatments should talk to their healthcare provider about fertility.
If you are concerned about any of the factors above, talk to your healthcare provider for specific advice for your health and wellbeing.
How does low sperm count affect fertility?
Getting pregnant with low sperm count can be more difficult, but it’s important to note that sperm count is only one factor in male fertility. The World Health Organization has developed guidelines for normal semen analysis.13 In addition to total sperm count, healthcare providers look at semen volume, sperm concentration, total motility (sperm making any movement), progressive motility (sperm moving in a straight line or a large circle), vitality and sperm morphology (the size and shape of sperm). If the sperm count is low, the chances of a single sperm fertilizing an egg are reduced.
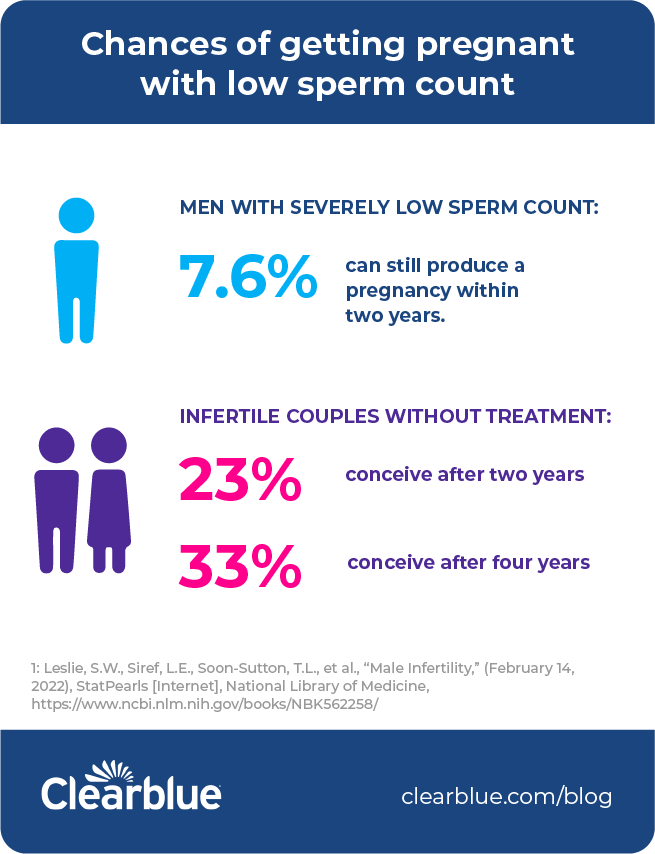
What are the chances of getting pregnant with low sperm count?
It is possible to get pregnant if your partner has low sperm count. Even with no treatment, studies have shown that 23% of infertile couples conceive after two years, and 33% conceive after four years. And 7.6% of men with severe low sperm count can still produce a pregnancy within two years with no treatment at all.1 Treatment can range from simple lifestyle changes (including the type of underwear worn) to surgery.
What treatment options can increase the chances of getting pregnant with low sperm count?
Talking to a healthcare provider is key for optimizing male fertility and sperm count. A semen analysis often provides a goldmine of information. If an analysis reveals low sperm count, a healthcare provider may suggest checking hormone levels in the blood, including testosterone, follicle-stimulating hormone (FSH), luteinizing hormone (LH) and prolactin.1 Genetic and chromosomal testing, ultrasounds and biopsies are also options.1 Sometimes these tests will result in multiple findings, highlighting issues with getting pregnant with low sperm count and motility.
Treatment options for low sperm count include:
- Lifestyle changes: According to studies, eat nutritious foods, exercise and try to lose some weight if obese. Stop smoking. Don’t use cannabis. Limit alcohol intake and don’t binge drink. Avoid environmental toxins. Also, heat can affect testicle sperm production, so avoid hot tubs and tight-fitting underwear.1,10
- Medication or counseling for sexual disorders: For pregnancy to occur, it’s important to have sex during the woman’s fertile window. An ovulation test can help with timing. Treating sexual disorders such as erectile dysfunction and retrograde ejaculation (when the semen enters the bladder instead of exiting the penis) can positively impact low sperm count.1
- Surgery: According to studies, a varicocelectomy (treating swollen varicoceles) can improve semen parameters in 60-70% of patients.1 Additional surgeries include a microsurgical vasovasostomy (to undo a vasectomy),2 a vasoepididymostomy (to treat epididymal blocks)2 and transurethral resection of the ejaculatory duct, or TURED (to treat an ejaculatory duct blockage).2
- Assisted reproductive techniques (ART): This includes IUI (intrauterine insemination), IVF (in vitro fertilization) and ICSI (intracytoplasmic sperm injection).2 According to the Urology Care Foundation, sperm retrieval methods include:2
- Testicular sperm extraction (TESE)
- Testicular fine needle aspiration (TFNA)
- Percutaneous epididymal sperm aspiration (PESA)
- Microsurgical epididymal sperm aspiration (MESA
- Additional therapies: Healthcare providers may suggest that men try clomiphene, an anti-estrogen that can increase FSH and LH levels; nasal testosterone gel; aromatase inhibitors; L-Carnitine; and antioxidants.1
What is azoospermia
When a man produces no sperm, it is called azoospermia.4 According to the National Institute of Child Health and Human Development, azoospermia is the cause of infertility in about 15% of men who are infertile.4 A diagnosis of azoospermia doesn’t mean pregnancy is impossible. Many of the treatment options that exist for low sperm count are the same as or similar to treatments that exist for no sperm count. Talk to your healthcare provider about different testing and treatment options.
Learning that low sperm count is affecting your chances of getting pregnant can feel disheartening. However, keep in mind that many couples experience infertility, whether from low sperm count or another reason — meaning that you’re not alone. And while low sperm count can be caused by several factors, just remember that for many of those causes, treatment options do exist.
Sources
- Leslie, S.W., Siref, L.E., Soon-Sutton, T.L., et al., “Male Infertility,” (February 14, 2022), StatPearls [Internet], National Library of Medicine, https://www.ncbi.nlm.nih.gov/books/NBK562258/
- “Male Infertility,” (accessed May 13, 2022), Urology Care Foundation, The Official Foundation of the American Urological Association, https://www.urologyhealth.org/urology-a-z/m/male-infertility
- “What are Varicoceles?” (accessed May 13, 2022), Urology Care Foundation, The Official Foundation of the American Urological Association, https://www.urologyhealth.org/urology-a-z/v/varicoceles
- “What are some possible causes of male infertility?” (January 31, 2017), Eunice Kennedy Shriver National Institute of Child Health and Human Development, https://www.nichd.nih.gov/health/topics/infertility/conditioninfo/causes/causes-male
- Hawksworth, D.J., Szafran, A.A., Jordan, P.W., Dobs, A.S., & Herati, A.S., “Infertility in Patients With Klinefelter Syndrome: Optimal Timing for Sperm and Testicular Tissue Cryopreservation,” (2018), Reviews in urology, 20(2), 56–62, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6168324/
- “Fertility in Men With CF,” (accessed May 13, 2022), Cystic Fibrosis Foundation, https://www.cff.org/fertility-men-cf
- “Y chromosome infertility,” (January 1, 2019), MedlinePlus, National Library of Medicine, https://medlineplus.gov/genetics/condition/y-chromosome-infertility/#causes
- “What is Testicular Trauma?” (accessed May 13, 2022), Urology Care Foundation, The Official Foundation of the American Urological Association, https://www.urologyhealth.org/urology-a-z/t/testicular-trauma
- La Vignera, S., & Vita, R., “Thyroid dysfunction and semen quality, (May 8, 2018), International Journal of Immunopathology and Pharmacology, https://doi.org/10.1177/2058738418775241
- Zhong, O., Ji, L., Wang, J. et al. “Association of diabetes and obesity with sperm parameters and testosterone levels: a meta-analysis, (October 16, 2021), Diabetology & Metabolic Syndrome (13)109, https://doi.org/10.1186/s13098-021-00728-2
- Krzastek, S.C., Farhi, J., Gray, M., & Smith, R.P., “Impact of environmental toxin exposure on male fertility potential,” (December 9, 2020), Translational Andrology and Urology, 9(6), 2797–2813, https://doi.org/10.21037/tau-20-685
- “Fertility Issues in Boys and Men with Cancer,” (February 24, 2020), National Cancer Institute, National Institutes of Health, https://www.cancer.gov/about-cancer/treatment/side-effects/fertility-men
- “WHO laboratory manual for the Examination and processing of human semen, Fifth Edition,” World Health Organization, https://www.who.int/docs/default-source/reproductive-health/srhr-documents/infertility/examination-and-processing-of-human-semen-5ed-eng.pdf




