Can you get pregnant on birth control?

This article discusses methods of birth control generally. For registered methods of birth control, and specifically for drug and medications, please always refer to product information and usage instruction.
Whether you’ve been using birth control for a couple of months or a decade plus, at some point you may begin to think about pregnancy. You likely have questions. Is it possible to get pregnant while using birth control? How long will it take for birth control to “clear out of your system”? And does taking birth control affect your fertility?
In short: if you are using birth control and thinking about trying to get pregnant, or if you’re thinking about starting birth control and know that you want to get pregnant in the near future, talk to your healthcare provider. It’s common knowledge that using contraception now won’t affect your chances of getting pregnant in the future, but the type of birth control you choose could affect the amount of time it takes to get pregnant if and when you do start trying. Communication with your doctor is key.
Your chances of getting pregnant on birth control1,2,3
How effective is birth control? Whether you’re new to birth control or you’ve been using it since you were a teen, you may have some questions about its efficacy. You’ve probably heard at least one story about someone who was using birth control but still got pregnant when they didn’t want to be.
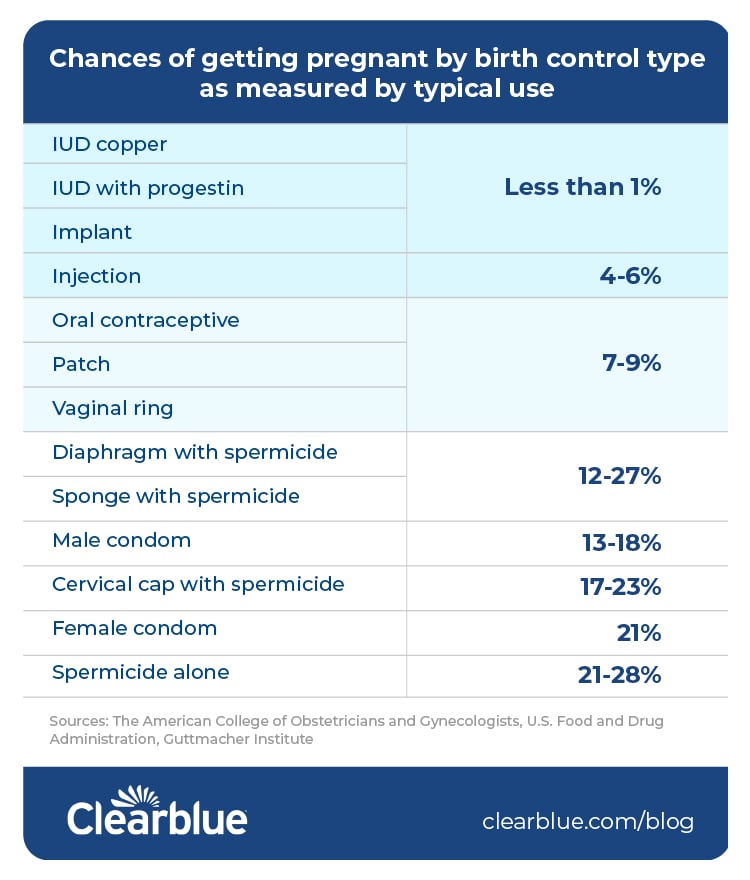
Research shows that no form of birth control is 100% effective, and different methods have different levels of effectiveness. For example, according to The American College of Obstetricians and Gynecologists, U.S. Food and Drug Administration and Guttmacher Institute, IUD effectiveness is statistically greater than birth control pill effectiveness.1,2,3
The Pearl Index is a commonly used method for reporting birth control efficacy. It looks at the number of pregnancies during one year of constant use of one type of birth control method out of a group of 100 people. Birth controls with higher efficacy rates have a lower Pearl Index.4
It’s also important to talk about how effectively you’re using your chosen form of birth control. It is common knowledge that correctly using birth control (like remembering to take an oral contraceptive daily, using condoms before their expiration date, etc.) impacts how well it can work. When looking at how effective a method could be for you, it’s important to consider how well it works with perfect (correct, every time) use, and with typical (average, including human error) use.
The chart below shows your chances of getting pregnant by birth control type as measured by typical use. Let’s take a closer look at what public studies say about birth control effectiveness.
Less than 1 pregnancy per 100 women per year:
- IUD copper: less than 1%
- IUD with progestin: less than 1%
- Implant: less than 1%
4 to 9 pregnancies per 100 women per year:
- Injection: 4 to 6%
- Oral contraceptives: 7 to 9%
- Patch: 7 to 9%
- Vaginal ring: 7 to 9%
12 to 28 pregnancies per 100 women per year:
- Diaphragm with spermicide: 12 to 17%
- Sponge with spermicide: 12 to 27%
- Male condom: 13 to 18%
- Cervical cap with spermicide: 17 to 23%
- Female condom: 21%
- Spermicide alone: 21 to 28%
How birth control affects your ability to conceive once you stop using it
Here’s the good news: According to a 2018 meta-analysis of 22 studies, contraception, regardless of how long you use it or what kind you use, doesn’t affect your ability to get pregnant once you stop using it.5 This meta-analysis was published in Contraception and Reproductive Medicine, and looked at 14,884 women who discontinued contraception use between 1985 and 2017. Within the first 12 months, 83.1% of these women reported getting pregnant.5
However, a 2020 study published by The BMJ found that the type of birth control you use may affect how long it could take you to conceive if you decide to start trying. According to The BMJ study, women who used the following contraception methods experienced, on average, these delays between stopping the use of birth control and conception:
- Injectables (five to eight cycles)
- Patches (four cycles)
- Oral contraceptives and rings (three cycles)
- IUDs and implants (two cycles) 6
Injectables contain the hormone depot medroxyprogesterone acetate (DMPA)7. According to ACOG, an injection of this hormone can keep you from getting pregnant for 13 weeks (which is why you need an injection four times a year).7 If you want to get pregnant in the near future, talk to your healthcare provider about what birth control method is best for you.
Fertility in the long run
Studies have shown that birth control should have no impact on your chances of getting pregnant once you stop using it. However, there are a number of different factors which can influence your fertility. It’s important to remember that getting pregnant can take longer than you think, regardless of contraception you may have used in the past. If you’re under 35 and have been trying to get pregnant for a year, over 35 and have been trying to get pregnant for over six months, or over 40 and interested in trying to get pregnant, talk to your healthcare provider about potential infertility concerns8.
There can be many reasons for infertility in men and women, including ovulation issues, PCOS, short luteal phases, early menopause, fibroids, endometriosis, age or issues with the sperm. What doesn’t cause infertility? Previously using birth control.5
According to the 2018 meta-analysis published in Contraception and Reproductive Medicine mentioned above, “resumption of fertility following cessation of contraception was not affected by use of contraception, type of contraception, duration of use and type of progesterone.”5
According to the American Society of Reproductive Medicine (ASRM), some types of birth control have additional benefits unrelated to pregnancy. For example, oral contraceptives can help treat irregular periods ; heavy or painful periods; endometriosis; PMS; acne; hirsutism (excess hair) and alopecia (hair loss).9 Per the ASRM, women who use birth control pills have also been found to have fewer cases of anemia, ovarian cancer and uterine cancer. 9
No matter why or when you started using birth control, if you’re thinking about trying to have a baby, talk to your healthcare provider. They will help you plan for this exciting next step.
Everything you want to know about the morning after pill

Accidents occasionally happen, and the morning after pill can be helpful for when they do. In this article, we answer your questions about the morning after pill and other forms of emergency contraception.
Sources
- “Effectiveness of Birth Control Methods,” (October 2021), The American College of Obstetricians and Gynecologists, https://www.acog.org/womens-health/infographics/effectiveness-of-birth-control-methods
- “Birth Control Chart,” (June 14, 2021), U.S. Food & Drug Administration, https://www.fda.gov/consumers/free-publications-women/birth-control-chart
- “Contraceptive Use in the United States,” (April 2020), Guttmacher Institute, https://www.guttmacher.org/fact-sheet/contraceptive-effectiveness-united-states
- "Birth Control Effectiveness & the Pearl Index Explained,” (March 2020), Natural Cycles, https://www.naturalcycles.com/cyclematters/birth-control-effectiveness-explained
- Girum, T., & Wasie, A., “Return of fertility after discontinuation of contraception: a systematic review and meta-analysis,” *July 23, 2018), Contraception and Reproductive Medicine, 3(9), https://doi.org/10.1186/s40834-018-0064-y
- Yland, J.J., Bresnick, K.A., Hatch, E.E., Wesselink, A.K., Mikkelsen, E.M., Rothman, K.J., et al., “Pregravid contraceptive use and fecundability: prospective cohort study,” (September 18, 2020) BMJ, https://www.bmj.com/content/371/bmj.m3966
- “Progestin-Only Hormonal Birth Control: Pill and Injection,” (October 2020), The American College of Obstetricians and Gynecologists, https://www.acog.org/womens-health/faqs/progestin-only-hormonal-birth-control-pill-and-injection
- “Treating Infertility,” (November 2020), The American College of Obstetricians and Gynecologists, https://www.acog.org/womens-health/faqs/treating-infertility
- “Noncontraceptive Benefits of Birth Control Pills,” (revised 2011), American Society for Reproductive Medicine, https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/noncontraceptive-benefits-of-birth-control-pills/

What are the early signs of pregnancy?
There are various symptoms that can indicate you might be pregnant, even if you might not experience any/all of them.




