The most advanced method to maximise the chances of getting pregnant naturally1-5a
Using the Clearblue® Fertility Monitor to identify the most fertile days can help women to conceive sooner than not using any method.1-5 It consists of a hand-held Monitor and disposable Test Sticks. It identifies changes in urine levels of two key hormones that control fertility, and is designed to accurately identify a woman’s entire fertile window2b (the days leading up to, and including day of ovulation). The Monitor has an intuitive touch screen display and other features that make it an effective and easy-to-use aid for women trying to conceive. Clearblue® is the number one brand recommended by OB-GYNs.c

The fertile window can be identified by tracking two key hormones
There are only a limited number of days in each cycle when a woman can get pregnant.6 Many women are unaware, or miscalculate the timing of their fertile days and may not be having intercourse at the best time in the cycle in order to maximize their chances of conceiving.
- The menstrual cycle is controlled by the anterior pituitary gonadotropins (follicle-stimulating hormone and luteinizing hormone, LH) and the gonadal sex hormones (estrogen and progesterone)7
- Plasma estradiol is the major physiological determinant of the onset of the fertile window; it stimulates secretion of cervical mucus that is favorable for the survival and transport of sperm. Estradiol levels gradually rise in the early stage of the woman’s cycle, reaching a threshold that triggers a sudden increase in LH – the LH surge8
- The LH surge is the best indicator of impending ovulation; it causes the dominant follicle to rupture and release a mature ovum. Ovulation typically occurs 24–36 hours after the LH surge, and will not occur in its absence.9
- Estrone-3-glucuronide (E3G) is a principal metabolite of estradiol which is recognised by the World health Organisation (WHO) as the best parameter for identification of the onset of the fertile phase10. Urinary levels of E3G correspond to the serum levels of estradiol.11
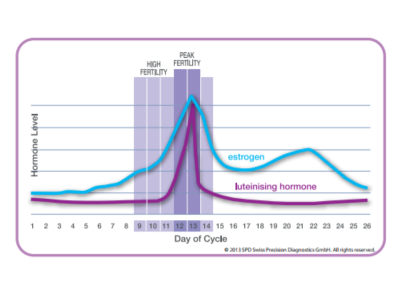
Schematic of typical hormone levels found in urine throughout the cycle.
The Clearblue® Fertility Monitor accurately identifies days of High and Peak fertility
The Clearblue® Fertility Monitor gives women comprehensive, personalized information that is unique to each cycle. It uses patented technology which has been developed into a unique dual-hormone assay for E3G and LH.

- The touch screen display guides a woman through her cycle; it will prompt the user when to perform tests by displaying ‘Test day’
- The user performs a test by using a Test Stick to obtain a urine sample, and then inserts the test stick into the Monitor to obtain a result
- The Test Sticks use monoclonal antibodies and optical technology to measure the levels of LH and E3G present in the urine. A sophisticated algorithm in the Monitor collects this information, along with menstrual cycle characteristics, and transforms it into a simple-to-understand indicator of fertility level

- Low is displayed on days when it is unlikely but not impossible that intercourse will result in pregnancy
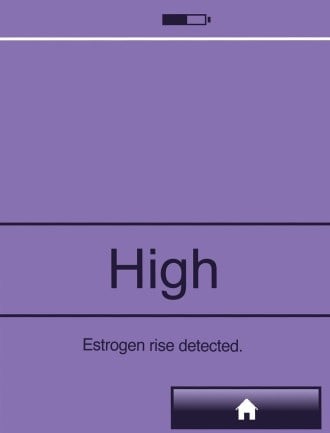
- High is displayed on the day the Monitor detects an elevated level of E3G and indicates that there is a high probability that intercourse at this time may lead to pregnancy. The Monitor then continues to display High on subsequent days until the detection of the LH surge. High will also be displayed for one day following the days of Peak Fertility as there is also a chance that pregnancy can occur on this day.

- Peak is displayed on the day, and subsequent day, of the Monitor detecting a surge in LH, which typically occurs 24–36 hours before ovulation, and indicates that the user is at the most fertile time in her cycle.
Tested extensively in clinical and laboratory studies:
- It accurately detected hormone levels, when compared with serum hormone levels6,12
- It was 99% accurate in detecting the LH surge, when tested using clinical samples13
- It has been shown to accurately predict ovulation compared with serum hormone measurements and vaginal ultrasound scans2,9
- The mean duration of the combined high and peak fertility days detected was 6.01 ± 2.33 days, in a laboratory analysis of daily urine samples from 352 menstrual cycles14
- In a study of 54 couples who were seeking conception assistance, the Monitor identified a median of seven fertile days; more than 60% of cycles had between 1 and 5 days of high fertility, prior to peak fertility, over four cycles.15
Additional information can be entered and saved in the Clearblue® Fertility Monitor
The user can also enter additional cycle information into the Monitor:
- Days and levels of menstrual bleeding
- Dates of intercourse; this data is useful to enable the user to track whether she has been having well-timed intercourse, she can then share this information with her healthcare professional if she does not become pregnant.
All information is displayed on a monthly summary screen and six-cycle summary chart
The Clearblue® Fertility Monitor displays key information collected in the previous six cycles on a cycle summary chart. The user can then share and discuss this information with their healthcare professional.
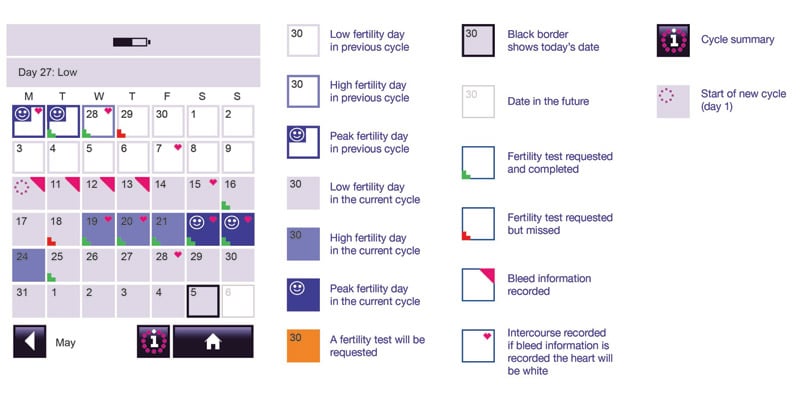
Example monthly summary screen and explanation of symbols
The cycle summary chart screen displays data from the previous six cycles in a graph format. It displays a summary of length of cycle and days of High and Peak fertility, together with records of intercourse on High and Peak days.
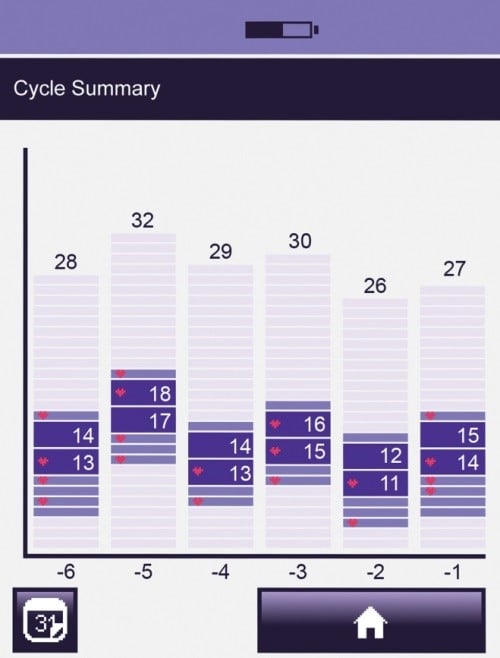
Example cycle summary chart
Additional user functionality
Additional user functions of the Clearblue® Fertility Monitor include:
- Option to set a PIN which the user will be asked to enter each time the Monitor is switched on, this helps to stop other people accessing her personal data
- The user can set an alarm to remind her when to test:

This symbol will be displayed in the information bar to confirm an alarm has been set - The Monitor will automatically set a testing window from 05.00 to 11.00 am (as urine tests need to be performed on first morning urine) and the user can only perform a test during this 6 hour window. However, the user can change the timing of this testing window if they wish.
The Clearblue® Fertility Monitor is:
- Accurate - 99% accurate at detecting the LH surge in urine13
- Unique - the only monitor to provide daily fertility status by measuring two urinary hormones – LH and E3G
- Effective - helps women to conceive soonera
- Adaptive - monitors individual hormone levels and adapts based on last six cycles of data, if available
- Personalized - allows women to enter additional personal information such as dates of menses and intercourse
- Easy to use - intuitive and easy to use touch screen
- Recommended - Clearblue® is the #1 ovulation brand recommended by OB-GYNsc
- aUsing the Clearblue® fertility Monitor to identify the most fertile days can help women get pregnant sooner than not using any method.
- bNumber of fertile days will vary. In a German study of 149 cycles, Monitor results correlated with serum hormone levels and ultrasound observed ovulation.6
- cData on file
- 1Robinson J., et al. Increased pregnancy rate with use of Clearblue® Easy Fertility Monitor. Fertility and Sterility. (2007) 87: 329–34.
- 2Wilcox AJ., et al. Timing of sexual intercourse in relation to ovulation. New England Journal of Medicine. (1995) 333: 1517–21.
- 3Robinson JE and Ellis JE. Mistiming of intercourse as a primary cause of failure to conceive: results of a survey on use of a home-use fertility monitor. CMRO (2007) 23: 301-306.
- 4Stanford JB, White GL and Hatasaka H. Timing Intercourse to Achieve Pregnancy: Current Evidence. American College of Obstetrics and Gynecologists (2002) 100: 1333-1341.
- 5Hilgers TW, Daly KD, Prebil AM and Hilgers SK. Cumulative pregnancy rates in patients with apparently normal fertility and fertility focused intercourse. Journal of Reproductive Medicine (1992) 37(10): 864-866.
- 6Behre HM., et al. Prediction of ovulation by urinary hormone measurements with the home use Clearblue® Fertility Monitor: comparison with transvaginal ultrasound scans and serum hormone measurements. Human Reproduction (2000) 12: 2478–2482.
- 7Martinez AR., et al. Prediction and detection of the fertile period: the markers. International Journal of Fertility. (1995) 40: 139–155..
- 8Burger HG. Estradiol: the physiological basis of the fertile period. International Journal of Gynecology and Obstetrics. (1989) Suppl 1: 5–9.
- 9Kerin JF., et al. Morphological and functional relations of Graafian follicle growth to ovulation in women using ultrasonic, laparoscopic and biochemical measurements. British Journal of Obstetrics and Gynaecology. (1981) 88: 81–90.
- 10World Health Organization. Temporal relationships between indices of the fertile period. Fertility and Sterility. (1983) 39: 647–654.
- 11Catalan R., et al. Correlation between plasma estradiol and estrone-3-glucuronide in urine during the monitoring of ovarian induction therapy. International Journal of Fertility. (1989) 34: 271–275.
- 12 Tanabe K., et al. Prediction of the potentially fertile period by urinary hormone measurements using a new home-use monitor: comparison with laboratory hormone analyses. Human Reproduction. (2001) 16: 1619–24
- 13Data on file: In laboratory testing, the Clearblue® Fertility Monitor detected the LH surge in 169/171 cycles, in agreement with a quantitative radioimmunoassay.
- 14Data on file. Laboratory Evaluation of Clearblue® Fertility Monitor System Performance; 90 women contributed up to 5 cycles of daily early morning urine samples where the Clearblue® Fertility Monitor system detected an LH surge, (352 cycles total) the range in cycle length was 22 to 40 days inclusive
- 15Bhiwandiwalla PP., et al. Assessment of the Clearplan Easy Fertility Monitor (CPEFM) in couples seeking conception assistance. Obstetrics and Gynecology. (2001) 97: 29S.

